A new model for driving patient engagement in healthcare
Supporting and empowering patients are objectives stated by nearly every life science company. Yet efforts to support patient engagement often fail to have the breadth and depth of impact companies aim for. So how can life science companies better engage patients? The answer lies in careful consideration of the patient mindset at specific critical points in their diagnostic and treatment journey. A leader in life science strategy, Putnam has developed innovative methods for quantifying patient emotional impact on the healthcare professional (HCP) decision-making process with the Integrative Affect Model (IAM). This model is not only a better way of capturing market insights with patients, but also a more effective way of helping life science companies engage with patients and providers. At Putnam, we are always striving to engage with patients in more impactful and meaningful conversations to assist them in becoming better stewards of their own care, especially when it comes to making healthcare decisions. The IAM allows us to understand when and how to engage with patients, positively impacting patients’ decisions.
Developing winning strategies in complex and rapidly evolving therapeutic markets starts with a superior understanding of the decision-making process that plays out between HCPs and patients. The two are intertwined as the HCP seeks to provide care and support and the patient seeks to pursue treatment options best aligned with their health and life objectives. Through this interaction the patient, and their caregivers, are simultaneously navigating the healthcare system and complicated emotions. The Integrated Affect Model provides a new and unique lens to evaluate needs and direct better engagement with patients. Timely and tailored patient engagement, informed by this model, can support more effective launches and help ignite new growth in established brands.
An evolution in integrated insights and reporting
Moving from a one-dimensional primary strategic insights method to an enhanced two-dimensional model, the IAM is a natural evolution of quantifying emotional impact.
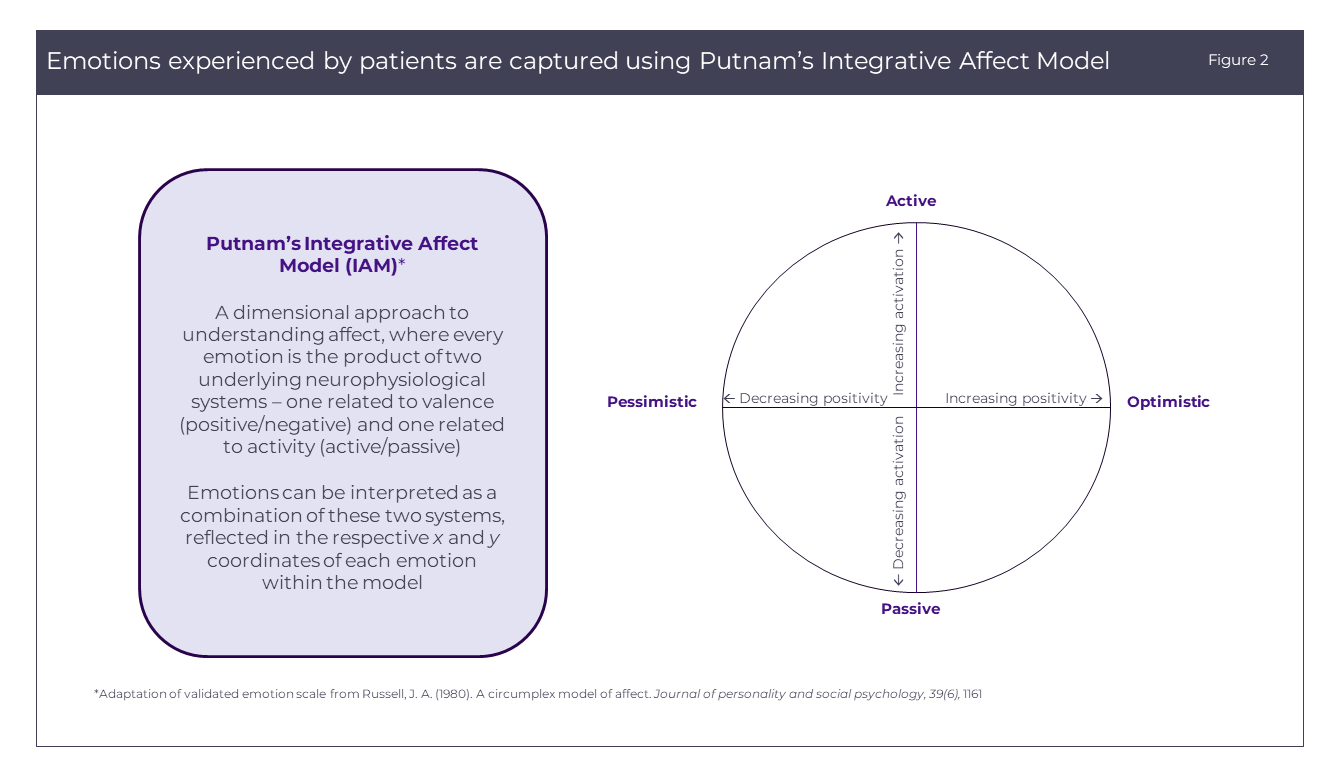
One of the biggest challenges in patient engagement is capturing emotion, be it emotions experienced in the past at diagnosis or in the present as the patient makes challenging treatment decisions. Patient research has historically captured patient affect (the set of emotional factors experienced by the patient) by selecting emotional keywords, which does not allow researchers to suitably anchor emotions to perceptions and behavior at each point throughout the patient journey. Through our expertise in the behavioral sciences and patient insights, we have developed a model for capturing emotion, based on a validated metric in affective research[1]. This allows a better understanding of the variability of emotion throughout the patient journey and more precisely targets opportunities for patient engagement.

The Integrative Affect Model
Putnam’s proprietary IAM takes a dimensional approach to understanding patient affect, where emotion is the product of two underlying neural systems, one related to valence (pleasant/unpleasant) and one related to activity (activation/deactivation). Emotions can then be interpreted as a combination of these two systems, reflected in the respective x and y coordinates, and tracked over time across the peaks and troughs of the patient journey. By pinpointing emotions experienced in these specific micro-moments, or critical moments in the patient experience where patients will be seeking answers and support, a brand can better mirror those emotions through more targeted and adaptive messaging and outreach to consumers.
How the Integrative Affect Model works
Patients are asked to select one emotion from each scale that best represents how they felt at a given time point (e.g., at diagnosis, first appointment with the oncologist, during first-line treatment, etc.). Scales are then plotted as axes on a heat map, where each square represents frequency of responses for each respective x and y coordinate. Squares that are absent of color represent emotions that did not accurately describe how patients felt. The more colored a square, the more these emotions accurately describe how patients felt in that moment.
Rather than depicting emotions experienced as one-dimensional bar charts, the ebb and flow of emotions across these micro-moments in time are better illustrated. Our model is adaptable for use across methodologies (and has already been used in both qualitative and quantitative research), sample sizes, and therapeutic areas.

A deeper understanding of HCP interactions with patients
By overlaying the IAM with key HCP decision points, we can also uncover a deeper understanding of the interactions between HCPs and their patients and how these critical moments may impact physician decision-making.
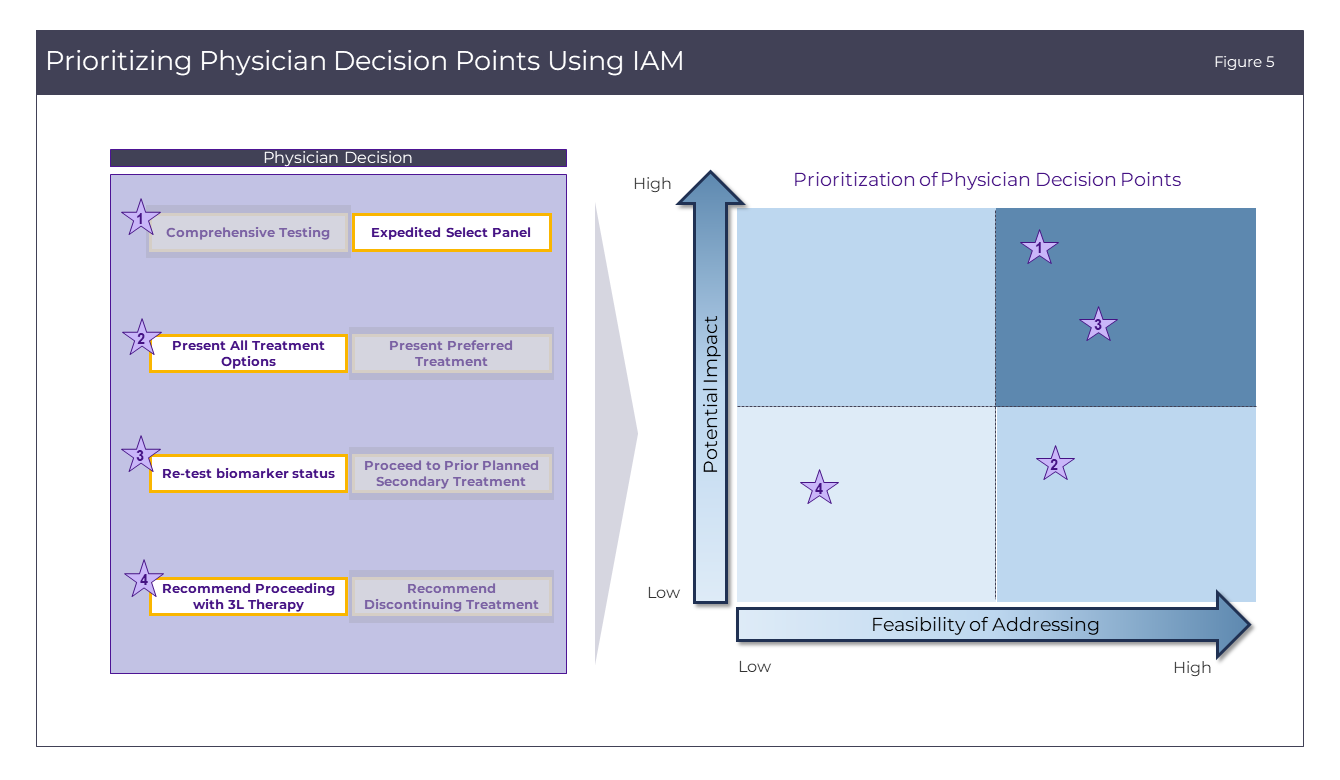
Through our primary strategic insights, we have seen how, even when physicians are the final decision-makers on treatment recommendations, their decisions are heavily influenced by the emotional state of their patients. For example, at the onset of symptoms, does patient anxiety track with the treating physician’s decision to order one or both types of biomarker tests based on which has the quickest turnaround vs. greater sensitivity? Does a patient’s determination to receive the best treatment lead physicians to introduce all potential treatment options upon diagnosis, or will a patient’s fear lead physicians to only present their top recommendation to avoid overburdening the patient? Understanding where patient affect may have the greatest potential to influence HCP decision-making allow us to create a more cohesive strategy between healthcare providers and their patients.

Prioritizing engagement strategies using the IAM
Finally, it is crucial to understand the potential impact of those physician decisions, and the underlying patient emotions, on brand performance. Using the Integrated Affect Model, one can also draw a more complete conclusion of how feasible it is to address different points of physician decision-making. Is it more likely to encourage doctors to convince patients that comprehensive biomarker testing is the best path towards developing a personalized path of care, or to ask doctors to present all treatment options to an overwhelmed and fearful patient? By conducting a rigorous assessment of the potential impact to brand as well as the feasibility of addressing the decision point, brand teams can prioritize the physician decision points for which messaging is most likely to have an effect.
Putnam delivers winning strategic guidance through deep understanding of critical moments in the patient experience where patients seek both answers and support. In addition to standard patient segmentations, we offer expertise in cognitive and behavioral primary strategic insights to better support our clients in reflecting those patient emotions in more tailored and innovative engagements – leading to enhanced patient experiences and stronger brand performance.
References:
- Russell, J. A. (1980). A circumplex model of affect. Journal of Personality and Social Psychology, 39(6), 1161.



